Thank you so much for the outpouring of caring. Reading all the notes made me teary and grateful for all of the wonderful people in my beautiful daughter’s life. I’ll try to update every day, but sometimes it might be hard.
Things are changing quickly. After a traumatic couple of days, Caitlin was relatively stable in the ICU yesterday. Late last night, I even texted a simple “things are good” to a few people.
But part of Caitlin, I think, believed that she “lost control” over the weekend, and caused herself to end up on ECMO. Yesterday she was trying to do everything she could to control her situation, control her life. She was talkative, questioning, in charge and speaking her mind, and also quite funny.
She’s always been her own advocate, but she pulled no punches. When someone did something wrong: “You should have known. Don’t do it again.” “I usually say please and thank you but I can’t waste the breath.” To the attending ICU doc who was part of the ECMO procedure: “I like you. You’re good.” To the annoying resident who started to examine her: “You just touched your hair, change your glove.” To the nurse last night: “You’re good. I bet you’re a Capricorn.” “I am,” he said. “I bet you’re good with money.” “I would be if I had some.”
But she wasn’t herself, spoke in a flat, blunt, odd way, and that was beginning to alarm me. Still, I reasoned, she had been through a lot. I hoped she would sleep and come back to herself. She did not sleep. Instead, she became increasingly hard to talk to and would not stop talking. She took my new brown notebook and began to write, constantly—- ideas for her care, new plans, instructions for all of us, lists, trying to account for every day, every hour. Her heart went into SVT again, and she had to be shocked again. By 4am, she still hadn’t slept and was no longer making sense. It wasn’t even like she was Caitlin.
Sleep deprivation on top of trauma. What a combination.
We had promised her we would stay close to her the first night, and we did, but by 5:30 am it was clear we were doing more harm than good. Nick went to sleep in the family room, where I’d managed to get about 6 hours “rest” on a chair. I went home and showered. I was almost back to the hospital when Nick said she still hadn’t slept and was still writing as fast as she could in the notebook and that the team thought it best we not see her for a while.
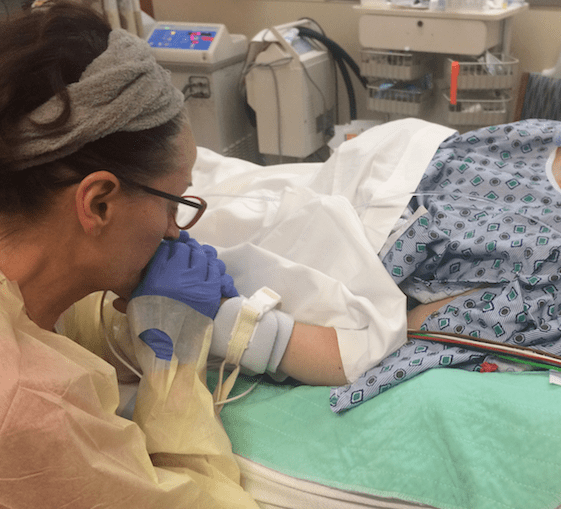
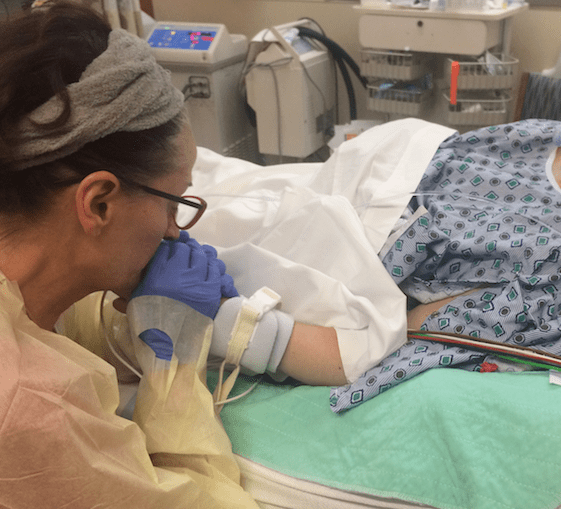
We talked to the attending about the fact that her condition was no longer stable. We talked about options. Shortly thereafter, the attending called us back and said the team had decided to intubate her. That allows her to breathe on a ventilator to rest her body/her lungs. Tomorrow they will put in a trach (which she would have likely gotten after transplant anyway.) The trach lets them have easy access between her body and the ventilator, and access to her airways. She’s having trouble coughing, so this will help. Tomorrow, they are also going to do a bronchoscopy, where they go into the lungs and clean them out. None of this is ideal but it’s now necessary, and it’s common, and it saves her life for now.
A while later, her wonderful nurse called (I need to clone this nurse) and explained that Caitlin was finally resting but told me, with honesty and compassion, about how out-of- control and combative Caitlin had become. I’ll spare the details but basically, the kitten had become a thrashing, panicky tiger. Erin, God love her, said, “Right before sedation, I told her, ‘Caitlin, I don’t care what you say or do. Right now, I’m going to save your life.'”
And that seemed to get through to her.
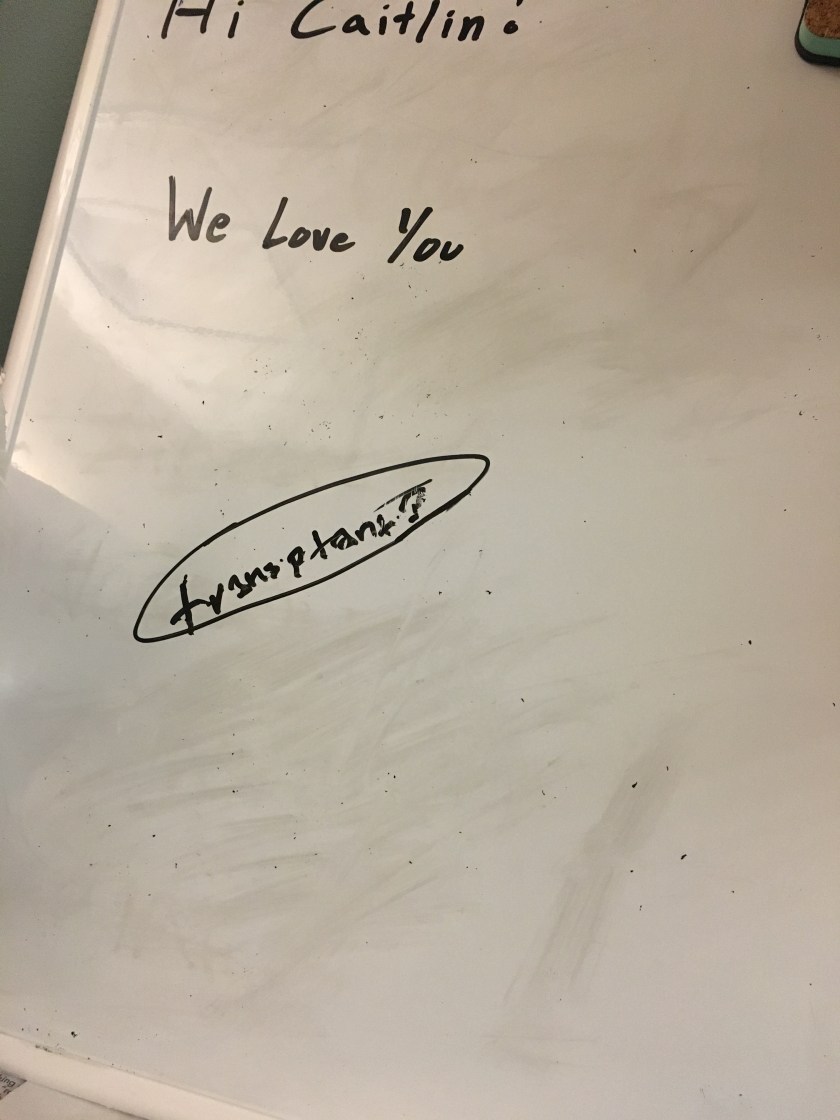
Now, on the vent, she can be a bit more sedated, and as comfortable as possible… and hopefully her new lungs her surgeons have promised will be inside of her soon.
I want to weep with gratitude for this hospital, the only one in the country that will accept such high-risk transplants, the people other hospitals have rejected because the transplants might fail and mess up their shining success statistics.
The good news? Remember yesterday I wrote about that other family from MA? The young CF woman had also been intubated and on ECMO and had even been on dialysis before transplant. Well, last night I went up to the terrible cafeteria because I was desperate for something to eat and there they were! The mother and daughter, the daughter on her feet, walking around ! 3 1/2 weeks after this same trauma, after transplant. I felt like I was seeing an angel.
–Maryanne